Deep Vein Thrombosis
What Is Deep Vein Thrombosis?
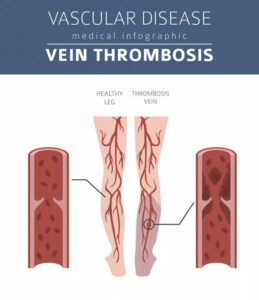
Deep vein thrombosis (DVT) is a disease that occurs when a blood clot forms in the deep vein system. DVT clots most common occur in the legs, although it can affect other parts of the body, such as the pelvis or arms.
Blood clots occur when blood thickens and clumps together. Deep vein thrombosis symptoms typically include swelling, discoloration, cramping, or warmth in the affected area or, sometimes, no signs at all. DVT can take a more severe turn if a blood clot in your vein travels up to your lungs and causes a pulmonary embolism.
Deep Vein Thrombosis Symptoms
DVT signs and symptoms usually form in one leg or arm. However, not everyone will experience DVT symptoms, and the condition may go undetected until examined by a physician. he most common deep vein thrombosis symptoms include:
- Swelling in the leg
- A feeling of warmth in the affected area
- Skin redness
- Pain or tenderness in your lower body, such as a cramp
DVT Causes And Risk Factors
DVT can form at any age as a result of anything that prevents the blood from circulating properly, such as prolonged periods of immobility, certain medications, surgery, or injury to a vein.
According to the CDC, close to 900,000 people are affected by either DVT or a pulmonary embolism (PE), or both, in the US each year. Many people experience deep vein thrombosis symptoms that resemble those of varicose veins, which often makes it difficult to diagnose DVT without an ultrasound.
The condition can also occur without any DVT symptoms, making it very important to learn the causes of DVT. This way, you can take preventative measures to decrease your risk of developing blood clots.
- A recent accident or surgery that requires lengthy bed rest: Blood clots can develop in veins damaged by surgery or trauma, or as a result of inflammation from an injury or infection.
- Having a blood-clotting disorder or a family history of these disorders: If a parent or sibling had DVT, you might be at greater risk of developing the condition. Moreover, some individuals have a genetic propensity that makes their blood clot more easily.
- Sitting for long periods, such as when driving or flying: Being immobile for long periods of time can impact your circulation. Blood clots can form in your lower legs if your calf muscles don’t move or contract for extended periods.
- Current or former smoker: Smoking affects circulation and blood clotting, which can increase your risk of DVT.
- Varicose veins: People with enlarged, bluish veins near the surface of the skin can be at risk for developing a clot in the deeper veins of their legs. If you have varicose veins, an experienced vascular specialist can assess your risk for deep vein thrombosis.
- Cancer: Different forms of cancer, such as breast, ovarian, pancreatic, bowel, and lung cancers, can increase substances in your blood that cause it to clot. Chemotherapy also increases the risk for DVT in individuals with cancer.
- Obesity: Being overweight puts pressure on the veins in the legs and pelvis, which can impact blood flow. The risk for DVT increases as the body mass index (BMI) rises.
- Pregnancy: Women who are pregnant or have recently given birth are more likely to develop DVT than other women. Although DVT during pregnancy is rare, the expanding uterus puts increased pressure in the veins of the pelvic area and legs, which can cause blood clots. Postpartum DVT can occur from damaged blood vessels in the pelvic area and uterus after giving birth.
- Over the age of 60 years old: Your risk of having DVT increases after the age of 40, nearly doubles with each succeeding decade, and peaks at age 60.
Deep vein thrombosis symptoms become dangerous if the blood clot breaks loose. Clots which break off can potentially travel through the bloodstream and land in the lungs — a condition called Pulmonary Embolism (PE). It’s important to talk to a vascular specialist if you notice any signs of DVT. They can perform an ultrasound to officially diagnose the disease.
DVT Complications
DVT is preventable and treatable. However, in some cases serious complications can develop, including pulmonary embolism.
Pulmonary Embolism (PE)
Deep vein thrombosis symptoms become dangerous if the blood clot breaks loose. Clots which break off can potentially travel through the bloodstream and land in the lungs — a condition called a Pulmonary Embolism (PE).
Be sure to act fast if you experience the following symptoms:
- Rapid heart rate
- Difficulty breathing
- Coughing up blood
- Feeling lightheaded or faint
- Chest pain or discomfort that worsens with a deep breath or cough
Seek immediate medical attention if a Pulmonary Embolism occurs. PE can be life-threatening and is a major risk factor for heart attack, so it’s critical to watch for the signs.
A blood clot is considered a medical emergency and demands immediate treatment because it can lead to a pulmonary embolism or other life-threatening condition.
It’s important to talk to a vascular specialist if you notice any signs of DVT, so they can perform an ultrasound to officially diagnose the disease.
Post-Thrombotic Syndrome (PTS)
PTS is a long-term complication of Deep Vein Thrombosis. It develops when a blood clot damages the valves in your veins and causes chronic pain, discomfort, and swelling. Symptoms of PTS can develop six months to two years after a blood clot forms, and can last for a lifetime.
Symptoms of PTS typically include:
- Skin discoloration
- Sores or ulcers on the skin
- Tingling and itching
- Pain and cramping
- Heaviness
- Swelling
Deep Vein Thrombosis Prevention
Being aware of common risk factors for DVT and making lifestyle changes are helpful to lower your risk of developing this condition, but they are not a guarantee.
One way to make sure you have a healthy circulatory system is to take care of your veins. The following lifestyle changes and healthy habits can help prevent DVT:
- Stay active: Blood clots commonly form while traveling. If you will be sitting for long periods, drink plenty of water. It’s also helpful if you walk or stretch your legs at least every two hours when traveling. If you cannot move around, try performing heel-to-toe exercises or flexing your feet to stretch out your calves. Regular exercise also can reduce your risk of developing deep vein thrombosis.
- Wear loose-fitting clothing: Tight-fitting garments can put pressure on your veins and circulatory system, which can affect the circulation in your legs. You should avoid wearing tight socks and clothes when traveling.
- Maintain a healthy weight: Increased weight puts additional pressure on your veins, which contributes to poor blood flow and the development of blood clots.
- Avoid smoking: One of the best ways to prevent a blood clot is to stop smoking or using any tobacco products. Smoking not only damages your lungs, but also your veins and arteries. Nicotine — an addictive chemical in cigarettes — can restrict the body’s blood flow and harden your arteries.
- Wear graduated compression stockings: Made of much stronger elastic fibers than typical hosiery, medical-grade compression stockings create significant pressure on your legs. This can help lessen deep vein thrombosis pain and discomfort, boost venous circulation, and decrease swelling. If advised by a doctor, you should wear compression socks continuously during the day and remove them when you go to sleep.
- Review your medications: Estrogen-containing medication, such as oral contraceptives or hormone replacement therapy, may increase risk for blood clots.
Deep Vein Thrombosis Treatment
If you notice enlarged, bulging, painful veins, you may have a vein disease that requires treatment. At Care Life Clinic, our vascular specialists are able to treat symptomatic vein disease to promote a healthy circulatory system in order to prevent the development of deep vein thrombosis.
Our doctors use minimally-invasive procedures to treat the source of your vein disease to reduce symptoms and prevent future health risks, such as DVT.
